 Getty Images
Getty Images
Around 50,000 Indians are killed by snakebites each year - roughly half of all deaths worldwide
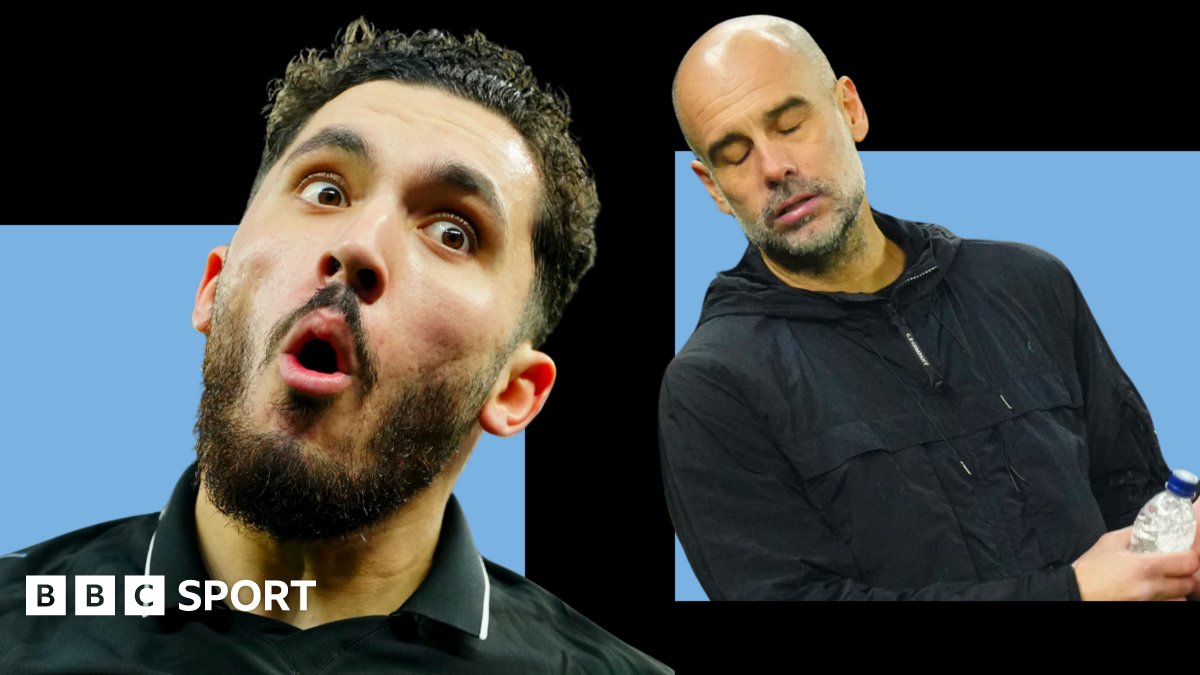
Devendra, who was a farmer in India, still remembers the moment a snake sank its fangs into his leg while he was picking mulberry leaves.
"I went to the hospital four days after I was bitten, when the pain became unbearable. But the delay cost me my leg," he says in a short film released by Global Snakebite Taskforce (GST), an initiative working to reduce deaths and injuries by snakebites.
But Devendra is still among the lucky few to have survived. According to the federal government, around 50,000 Indians are killed by snakebites each year - roughly half of all deaths worldwide. Some estimates suggest the toll could be even higher: between 2000 and 2019, India may have seen as many as 1.2 million deaths, an average of 58,000 per year, a 2020 study said.
Now, a new report by GST has found that 99% of healthcare workers in India face challenges administering antivenom - the life-saving antibodies that neutralise toxins in venom. Researchers surveyed 904 medical professionals across India, Brazil, Indonesia and Nigeria, the countries most affected by snakebites, and found similar barriers: poor infrastructure, limited access to antivenom and insufficient training.
Nearly half of the professionals reported that delays in treatment had led to serious complications in their patients, including amputations, surgeries or lifelong mobility problems.
It also states that snakebites disproportionately affect poor rural communities in low and middle-income countries.
 Strike Out Snakebite
Strike Out Snakebite
Devendra's leg had to be amputated after he was bitten by a snake while he was picking mulberry leaves
In India, a high concentration of snakebite deaths and injuries are reported in the central and eastern regions, says Dr Yogesh Jain, a GST member and a practitioner in the central Chhattisgarh state. He adds that people working in farms, including those from poor tribal communities, remain most vulnerable.
In 2024, India launched the National Action Plan for Prevention and Control of Snakebite Envenoming (NAPSE) with an aim to halve snakebite deaths by 2030. The plan focuses on better surveillance, improved antivenom availability and research, enhanced medical capacity and public awareness campaigns.
Experts agree it is a step in the right direction, but implementation has been inconsistent.
"In India, snakebites are seen as a poor person's problem," Jain says. "That's why there isn't enough outrage or action over these completely avoidable deaths. When it comes to treating snakebites, every second counts."
He explains that snake venom enters the bloodstream within minutes, attacking nerves, cells, or the circulatory system depending on the species. Delays in antivenom administration can result in respiratory failure, paralysis, irreversible tissue damage, or organ failure.
Yet, delays in hospitalisation are common in rural India where bad roads, far-flung hospitals and a dearth of ambulance services prevent timely treatment.
Last September, a pregnant woman in Gujarat state reportedly died on the way to a hospital after her family had to carry her in a cloth sling for 5km (3 miles) because no vehicle could reach their hamlet.
Jain says that some states are trying to improve access by stocking antivenom in primary and community health centres. But administering it correctly remains a major challenge.
Many health workers are not trained professionals and fear giving antivenom because patients can sometimes develop adverse reactions.
"The antivenom is mixed with saline and injected intravenously over an hour, but many centres aren't equipped to manage the side-effects," Jain says.
Another problem, he adds, is that many people in rural India still rely on faith healers or local medicinal practices and go to hospitals only when their symptoms worsen, which can be lethal.
 The Liana Trust
The Liana Trust
Gerry Martin's The Liana Trust has been researching antidotes for bites by regional snake species
Gerry Martin, co-founder of The Liana Trust, which works to reduce human-snake conflict in Karnataka state, says another major hurdle is the availability of high-quality antivenom.
Currently, India has antivenom that only protects against the "big four" snakes - the spectacled cobra, common krait, Russell's viper and the saw-scaled viper - which are believed to be responsible for a majority of the bites. The antivenom is produced by injecting venom from these snakes into horses, whose antibodies are then used as treatment for humans, Martin explains.
But there are dozens of other poisonous snake species for which India does not have targeted antivenom. These include the green pit viper commonly found in the northern state of Himachal Pradesh, the Malabar pit viper and hump-nosed pit viper found in southern states and many other species in the north-eastern states.
A study by Aiims (All India Institute of Medical Sciences) in Jodhpur, Rajasthan, last year highlighted the problem. It found that when antivenom used to treat bites by saw-scaled vipers was administered to 105 snake bite patients (where the species remained unknown), two-thirds did not respond well to treatment.
The study concluded that there was an urgent need for "region-specific antivenom in western India".
For the past five years, The Liana Trust has been studying venoms from species beyond the big four to develop antidotes to them. But progress has been slow, Martin says, because the process is labour-intensive and time-consuming.
He called on states to emulate the 2024 order from the government of the southern state of Karnataka which made snakebites "a notifiable disease" - making it compulsory for health professionals to report it to the authorities - to combat under-reporting.
Jain agrees. "Snakebite deaths start where political will ends," he says.
"Governments should ensure that poor people don't get poor health systems. They deserve better."

 2 hours ago
1
2 hours ago
1